
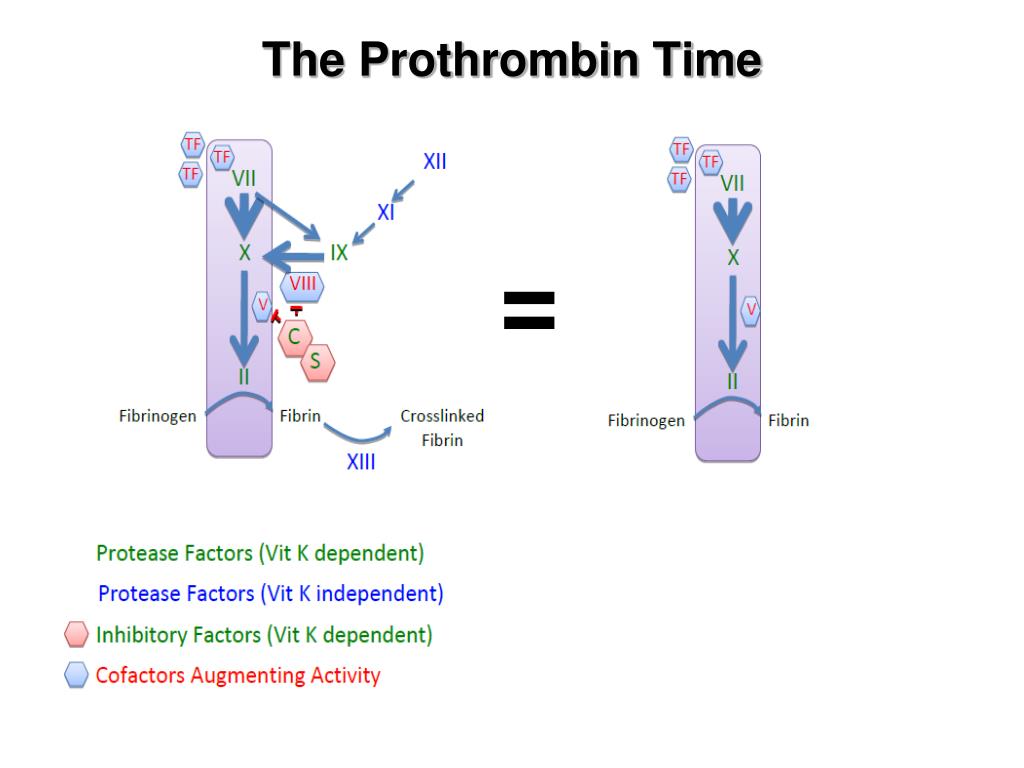
VKA therapy inhibits factors II, VII, IX, and X and causes a prolonged PT.DIC causes a system-wide activation of coagulation, depleting available coagulation factors leading to an increase in PT.Disseminated Intravascular Coagulation (DIC).Inherited diseases that lead to a decreased production of factors II, V, IX, and X will lead to a prolonged PT.Potential causes that can lead to decreased vitamin K levels include malnutrition, prolonged antibiotic use, and impairments with fat absorption. A deficiency in vitamin K will lead to a decrease in these factors and prolong PT. Vitamin K is a necessary component in factors II, VII, IX, and X.A decreased production of coagulation factors leads to prolonged PT and physical manifestations that can include petechiae and easy bruising. Liver disease or liver dysfunction leads to a decreased production of most coagulation factors.Assessment of liver synthesis function and to calculate the model for end-stage liver diseases (MELD) score in liver disease.Obtaining baseline value before initiating anticoagulation therapy.Diagnosing disseminated intravascular coagulation (DIC).Monitoring vitamin K-antagonists (VKA) such as warfarin is the most common indication for PT.Clot formation can then be detected mechanically or optically depending on the instrumentation used. Once the blood sample is ready to be tested, calcium chloride is then added to restore the calcium required for coagulation activation. The tube should not be shaken to avoid hemolysis that would lead to inaccurate results. The tube is then gently inverted a few times to mix the sodium citrate solution with the blood.
#P t inr normal range full
Tube filling must be within 90 percent of the full collection volume with blood to sodium citrate ratio of 9 to 1. This chelation keeps the blood sample in stasis until ready to be tested. Sodium citrate serves to chelate the calcium in the blood sample and prevents the activation of the coagulation cascade. Phlebotomists collect venous blood samples in plastic tubes with a light blue top that contains 3.2% sodium citrate. However, blood samples may also be obtained from indwelling intravenous lines when necessary.

Standard percutaneous phlebotomy is the recommended method used to collect venous blood samples. Coagulation tests must be performed using plasma samples and not serum as clotting factors get removed in serum preparations. Although point-of-care devices have been shown to underestimate hemostatic abnormality, point-of-care devices are generally reliable in non-emergency settings. With point-of-care devices, monitoring anticoagulation therapy can take place at thrombosis centers, primary care provider offices, and even by the patients themselves. With increased prescribing of vitamin K-antagonists (VKAs) like warfarin, point-of-care devices have also been more convenient for patients and general practitioners to monitor medication effectiveness.
POC devices are of great value in the emergency and operating room settings where clinical diagnosis and intervention are time-sensitive. However, due to the high turnaround time of up to 90 minutes, point-of-care (POC) devices, with a turn-around time of approximately 5 minutes, are becoming more desirable. Standard laboratory coagulation-based testing has traditionally been used to obtain measurements of PT to ensure reliable results. The INR represents the ratio of the patient's PT divided by a control PT value obtained by using an international reference thromboplastin reagent developed by the WHO. Due to this variability, the World Health Organization (WHO) introduced the international normalized ratio (INR) and has become the standard reporting format for PT results. Many different preparations of thromboplastin reagents are available which can give different PT results even when using the same plasma. PT measures the time, in seconds, for plasma to clot after adding thromboplastin, (a mixture of tissue factor, calcium, and phospholipid) to a patient's plasma sample. More specifically, PT is used to evaluate the extrinsic and common pathways of coagulation, which would detect deficiencies of factors II, V, VII, and X, and low fibrinogen concentrations. Prothrombin time (PT) is one of several blood tests routinely used in clinical practice to evaluate the coagulation status of patients.


 0 kommentar(er)
0 kommentar(er)
